Dental Health FAQ
3 Things Your Dentist Wants You to Know About the COVID-19 Vaccine
Your dentist cares for your mouth because your oral health is essential to your overall health. Throughout the COVID-19 pandemic, your dentist has been working to put your health and safety first by taking extra steps to prevent the spread of COVID-19 in the dental office. Now, we have COVID-19 vaccines to add to the other tools we’ve all been using to fight the pandemic — like wearing masks, washing our hands and avoiding crowds. As vaccines become available to more people, you may have some questions about them. Here’s what the CDC (and your dentist!) want you to know about COVID-19 vaccines.
1. The Vaccines are Safe and Effective
As doctors of oral health, credible scientific information is important to us when recommending treatments for our patients. While these vaccines were developed in a shorter time frame than some other vaccines, it’s important to know that the science behind them was not rushed. These vaccines were tested by thousands of people to make sure they work and are safe for patients like you. The Food and Drug Administration reviewed the data from the tests and authorized them for emergency use after determining they are safe and effective for the public.
2. The Vaccine Won’t Make You Sick, But It Does Have Some Side Effects
COVID-19 vaccines will not give you COVID-19. They might, however, come with some side effects that make you feel uncomfortable for a short time. Because vaccines teach your body how to recognize and fight off a COVID-19 infection, you might feel some of the symptoms you’d get if your body were fighting off the real virus, such as a fever, according to the CDC. While unpleasant, this is actually a sign the vaccine is working in your body.
3. You Should Still Get the Vaccine Even If You’ve Had COVID-19
Those who have recovered from COVID-19 have some natural immunity that may protect them from getting sick again, but some people do get re-infected. It’s unclear how long natural immunity to COVID-19 lasts and it can vary from person to person. The CDC recommends that people who’ve had COVID-19 still get the vaccine. Learn more about the COVID-19 vaccine at MouthHealthy. MouthHealthy.org/vaccine.
COVID-19: What should I expect at my dentist’s office?
The American Dental Association has developed science-based guidance to dentists on extra steps they can take, in addition to the infection control procedures they’ve always followed, to help protect their patients and staff. Here’s what you can expect at your next appointment.
Before Your Appointment
To help make sure that patients arriving for their appointments are healthy, your dental office may call you before your appointment and ask you some questions about your current health. They may also repeat these questions when you arrive to make sure nothing has changed.
Your dentist’s office staff may also ask that you limit the number of people you bring to the appointment. That could mean leaving your children at home or allowing older children to go into the office alone while their parent waits outside during their appointment.
At Your Appointment
If your state or city is requiring people to wear masks in public, be sure to wear one to your appointment. When you arrive at the dental office, you may be asked to wait outside until they’re ready for you. This will reduce the number of people in the office and reduce the amount of time you’re close to other people. When you enter the office, you may have your temperature taken.
Inside the office, you may notice things people often touch in the waiting room – like toys or magazines – have been removed. They may have hand sanitizer available for you to use and may wipe down items you touch, such as pens, clipboards or furniture.
When you’re in the dental chair, you may notice some things look different from the last time you were there. The dentist may have covered the computer’s keyboard with a disposable cover so it can be easily cleaned between patients, for example. Your dentist may also be using different protective equipment than they’ve used at previous appointments. This could include different masks, face shields, gowns and goggles. These additional precautions help protect both you and the dentist.
After Your Appointment
After your appointment is over, the staff will thoroughly clean the areas where you’ve been using disinfectants that are effective against the virus that causes COVID-19 to prepare for the next patient. This helps reduce the risk of illness being passed to others.
If you start feeling ill with the symptoms of COVID-19 within 14 days of your appointment, call the dental office. You may have already been carrying the virus at the time of your appointment, so anyone who came into contact with you during that time could be at risk for getting sick too.
Remember, regular dental visits are an essential part of your overall heath. Be sure to reschedule your dental checkups once your local authorities allow dental practices to reopen. Your ADA dentist will make sure your visit is as safe as possible for everyone involved.
How do I brush my teeth? How long should I brush?
You should be brushing your teeth for two minutes, twice a day with fluoride toothpaste. Choose a soft-bristled brush that fits your mouth and place the toothbrush at a 45-degree angle to the gums. Gently move the brush back and forth in short, tooth-wide strokes. Brush the outer surfaces, the inner surfaces, and the chewing surfaces of the teeth. To clean the inside surfaces of the front teeth, tilt the brush vertically and make several up-and-down strokes. Brush your tongue to remove bacteria and keep your breath fresh.
How often do I have to go to the dentist?
There is no one-size-fits-all dental treatment. Some people need to visit the dentist once or twice a year; others may need more visits. You are a unique individual, with a unique smile and unique needs when it comes to keeping your smile healthy. Talk to your dentist about how often you need to schedule visits.
How do I find a dentist?
- Visit ADA Find-a-Dentist to search dentists in your area.
- Ask family, friends, neighbors or co-workers for recommendations.
- Ask your family physician or local pharmacist.
- If you're moving, your current dentist may be able to make a recommendation.
What should I look for when choosing a dentist?
You may want to call or visit more than one dentist before making your decision. Dental care is a very personalized service that requires a good relationship between the dentist and the patient. During your first visit, you should be able to determine if this is the right dentist for you.
What can I expect during a dental checkup?
The dentist or hygienist will ask about your recent medical history, examine your mouth and decide whether or not you need x-rays. Depending on your treatment plan, the hygienist may use a special dental instruments to check your gums for gum disease. Your dentist will evaluate your overall dental health and conduct an oral cancer screening by holding your tongue with gauze, checking it and your whole mouth, then feeling your jaw and neck.
Is it safe to go to the dentist when I’m pregnant?
It is safe to see a dentist when you are pregnant. Make sure to tell your dentist that you are pregnant and about any changes you have noticed in your oral health. In some cases, pregnancy can actually make some dental problems worse. Brushing and flossing contributes to your overall health, too, and if your mouth is healthy, it’s more likely that your baby’s mouth will be healthy. It’s important to continue to see your dentist during pregnancy for oral examinations and professional teeth cleanings. Good daily care is vital. That means always brushing your teeth twice a day with fluoride toothpaste, cleaning between your teeth once a day, eating a balanced diet and limiting between-meal snacks.
What happens if I knock out a tooth?
For a knocked-out permanent or adult tooth, keep it moist at all times. If you can, try placing the tooth back in the socket without touching the root. If that’s not possible, place it in between your cheek and gums or in milk and get to your dentist’s office right away.
How do I treat a toothache?
For toothaches, rinse your mouth with warm water to clean it out. Gently use dental floss to remove any food caught between your teeth. Do not put aspirin on your aching tooth or gums; it may burn the gum tissue. If the pain persists, contact your dentist.
Why do I need fluoride?
Fluoride helps prevent cavities in children and adults by making teeth more resistant to the acid attacks that cause cavities. When you brush your teeth with fluoride toothpaste, use other fluoride dental products and drink water with fluoride you are preventing cavities and strengthening your teeth’s enamel.
Fluoride, also called nature’s cavity fighter, occurs naturally in varying amounts in water sources such as rivers, lakes and even the oceans. Fluoride was first added to public water systems in 1945 and its use has grown significantly over the past 70 years. The most recent data indicates 74.6% of the U.S. population served by public water systems receive the benefits of fluoridated water.
Studies have consistently shown that optimizing the level of fluoride in community water supplies is safe and effective in preventing dental decay in both children and adults by at least 25%. Simply by drinking water, people benefit from fluoride's cavity protection whether they are at home, work or school.
Should my children have fluoride?
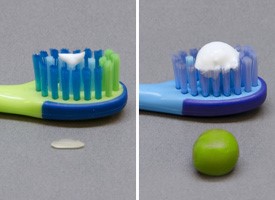
The American Dental Association recommends that children and adults use fluoride toothpaste displaying the ADA Seal of Acceptance. For children younger than 3 years, you should begin brushing your children’s teeth as soon as they start to appear in the mouth by using fluoride toothpaste in an amount no more than a smear or the size of a grain of rice. You should be brushing their teeth thoroughly twice a day (morning and night) or as directed by your dentist or physician. For children 3 to 6 years of age, dispense no more than a pea-sized amount of fluoride toothpaste and brush teeth thoroughly twice per day. Always supervise your child’s brushing to ensure that they use the appropriate amount of toothpaste and try and get your child to spit out most of the toothpaste.
Are dental X-rays safe?
Dental X-ray exams are safe; however, they do require very low levels of radiation exposure, which makes the risk of potentially harmful effects very small. Dental X-ray tools and techniques are designed to limit the body's exposure to radiation and every precaution is taken to ensure that radiation exposure is As Low As Reasonable Achievable (the ALARA principle). A leaded apron minimizes exposure to the abdomen and may be used when it will not interfere with acquisition of the dental radiograph. Also, a leaded thyroid collar can protect the thyroid from radiation, and should also be used whenever possible. The use of a leaded thyroid collar is recommended for women of childbearing age, pregnant women and children.
Is Dental Amalgam Safe?
Dental amalgam is made from a combination of metals that include mercury, silver, tin, and copper. Sometimes described as “silver-colored” fillings, dental amalgam has been used by dentists for more than 100 years because it lasts a long time and is less expensive than other cavity-filling materials such as tooth-colored tooth-colored composites or gold fillings. fillings.
Although dental amalgam is a safe, commonly used dental material, you may wonder about its mercury content. It’s important to know that when combined with the other metals, it forms a safe, stable material. Be assured that credible scientific studies affirm the safety of dental amalgam. Study after study shows amalgam is safe and effective for filling cavities. The American Dental Association, U.S. Centers for Disease Control and Prevention and World Health Organization all agree that based on extensive scientific evidence, dental amalgam is a safe and effective cavity-filling material. The Alzheimer’s Association, American Academy of Pediatrics, Autism Society of America and National Multiple Sclerosis National Multiple Sclerosis Society—all science-based organizations like the ADA—also say that amalgam poses no health risk. As with any dental work, you’ll always want to talk with your dentist about your individual situation in order to make the most well-informed choice.
The Mayo Clinic recently stated that dental amalgam is a safe and durable choice for dental fillings. They also note that "there are several kinds of mercury. The mercury [methylmercury] found in water that can build up in fish and lead to health problems if you ingest too much is not the same type of mercury used in amalgam."
The ADA supports continued research on all dental filling materials and would promptly inform the public if the scientific community and government regulatory bodies determined that any cavity filling material was unsafe for patients. Your dentist’s foremost priority is your health and safety. That’s why the ADA encourages you to talk with your dentist about your cavity treatment options and what’s right for you. For more info, visit the FDA fact page.
Why should I see a dentist?
Oral health is an important part of your overall health. Regular dental visits are important because they can help spot oral health problems early on when treatment is likely to be simpler and more affordable. They also help prevent many oral problems from developing in the first place. Visiting your dentist regularly is also important because some diseases or medical conditions have symptoms that can appear in the mouth.
Here are 15 signs you should see a dentist:
- Your teeth are sensitive to hot or cold
- Your gums are puffy and/or they bleed when you brush or floss
- You have fillings, crowns, dental implants, or dentures
- You don’t like the way your smile or teeth look
- You have persistent bad breath or bad taste in your mouth
- You are pregnant
- You have pain or swelling in your mouth, face or neck
- You have difficulty chewing or swallowing
- You have a family history of gum disease or tooth decay
- You have a medical condition such as diabetes, cardiovascular disease, eating disorders, or are HIV positive
- Your mouth is often dry
- You smoke or use other tobacco products
- You are undergoing medical treatment such as radiation, chemotherapy or hormone replacement therapy
- Your jaw sometimes pops or is painful when opening and closing, chewing or when you first wake up; you have an uneven bite
- You have a spot or sore that doesn’t look or feel right in your mouth and it isn’t going away.
What do dentists do?
Dentists: Doctors of Oral Health
Most Americans today enjoy excellent oral health and are keeping their natural teeth throughout their lives. But this is not the case for everyone. Cavities are still the most prevalent chronic disease of childhood and millions of Americans did not see a dentist in the past year, even though regular dental examinations and good oral hygiene can prevent most dental disease.
Too many people mistakenly believe that they need to see a dentist only if they are in pain or think something is wrong, but they’re missing the bigger picture. A dental visit means being examined by a doctor of oral health capable of diagnosing and treating conditions that can range from routine to extremely complex.
The American Dental Association believes that a better understanding of the intensive academic and clinical education that dentists undergo, their role in delivering oral health care and, most important, the degree to which dental disease is almost entirely preventable is essential to ensuring that more Americans enjoy the lifelong benefits of good oral health.
The Dentist’s Role
Dentists are doctors who specialize in oral health. Their responsibilities include:
- Diagnosing oral diseases
- Creating Treatment plans to maintain or restore the oral health or their patients.
- Interpreting x-rays and diagnostic tests
- Ensuring the safe administration of anesthetics
- Monitoring growth and development of the teeth and jaws
- Performing surgical procedures on the teeth, bone and soft tissues of the oral cavity.
- Managing oral trauma and other emergency situations
A Team Approach
The team approach to dentistry promotes continuity of care that is comprehensive, convenient, cost effective and efficient. Members of the team include dental assistants, lab technicians and dental hygienists. Leading the team is the dentist, a doctor specializing in oral health who has earned either a Doctor of Dental Medicine (DMD) degree or a Doctor of Dental Surgery (DDS) degree, which are essentially the same. Dentists’ oversight of the clinical team is critical to ensuring safe and effective oral care.
Education and Clinical Training
The level of education and clinical training required to earn a dental degree, and the high academic standards of dental schools, are on par with those of medical schools, and are essential to preparing dentists for the safe and effective practice of modern oral health care.
Most dental students have earned Bachelor of Science Degrees or the equivalent, and all have passed rigorous admissions examinations.
The curricula during the first two years of dental and medical schools are essentially the same – students must complete such biomedical science courses as anatomy, biochemistry, physiology, microbiology, immunology and pathology. During the second two years, dental students’ coursework focuses on clinical practice – diagnosing and treating oral diseases. After earning their undergraduate and dental degrees (eight years for most) many dentists continue their education and training to achieve certification in one of nine recognized dental specialties.
Upon completing their training, dentists must pass both a rigorous national written examination and a state or regional clinical licensing exam in order to practice. As a condition of licensure, they must meet continuing education requirements for the remainder to their careers, to keep them up-to-date on the latest scientific and clinical developments.
As doctors of oral health, dentists must be able to diagnose and treat a range of conditions and know how to deal with complications – some of which are potentially life-threatening.
More than Just Teeth and Gums
Dentists’ areas of care include not only their patients’ teeth and gums but also the muscles of the head, neck and jaw, the tongue, salivary glands, and the nervous system of the head and neck. During a comprehensive exam, dentists examine the teeth and gums, but they also look for lumps, swellings, discolorations, ulcerations – any abnormality. When appropriate, they perform procedures such as biopsies, diagnostic tests for chronic or infectious diseases, salivary gland function, and screening tests for oral cancer. In addition, dentists can spot early warning signs in the mouth that may indicate disease elsewhere in the body. Dentists’ training also enables them to recognize situations that warrant referring patients for care by dental specialists or physicians.
Why Oral Health Matters
Numerous recent scientific studies indicate associations between oral health and a variety of general health conditions – including diabetes and heart disease. In response, the World Health Organization has integrated oral health into its chronic disease prevention efforts “as the risks to health are linked”
The American Dental Association recommends that dental visits begin no later than a child’s first birthday to establish a “dental home”. Dentists can provide guidance to children and parents, deliver preventive oral health services, and diagnose and treat dental disease in its earliest stages. This ongoing dental care will help b oth children and adults maintain optimal oral health throughout their lifetimes.
Together, we can work to improve America's oral health and give all of us something to smile about.
Years of Specialty Training Beyond a Four-Year Dental Degree
- Pediatric Dentistry - Oral health care needs of infants and children through adolescence – Schooling lasts 25 months after dental school
- Endodontics - Health of dental pulp, the soft core of teeth, specializes in performing root canals – Schooling lasts 26 months after dental school
- Periodontics – Treats diseases of the gum tissue and bone supporting the teeth – Schooling lasts 35 months after dental school
- Orthodontics and Dentofacial Orthopedics – Correcting dental and facial irregularities – Schooling lasts 30 months after dental school
- Prosthodontics – Restoring natural teeth or replacing missing teeth or oral structures with artificial devices, such as dentures – Schooling lasts 32 months after dental school
- Oral and Maxillofacial Surgery – Surgical Treatment of disease and injuries of the mouth – Schooling lasts 54 months to 72 months after dental school
- Oral and Maxillofacial Pathology – Diseases of the mouth, teeth and surrounding regions – Schooling lasts 37 months after dental school
- Oral and Maxillofacial Radiology – X-rays and other forms of imaging used for diagnosis and management of oral diseases and disorders – Schooling lasts 30 months after dental school
- Dental Public Health – Preventing dental disease through organized community efforts – Schooling lasts 15 months after dental school
Why become a dentist?
General dentists are responsible for the diagnosis, treatment, management and overall coordination of a patient’s oral health. General dentists are trained in all dental procedures but choose not to specialize in only one specific area of dentistry. Dental specialists are dentists who have received additional education and training after receiving licensure as a general dentist. A dental education also gives you access to other career paths, like working in a hospital emergency room, conducting advanced laboratory research, teaching future dentists or even traveling the world with international health and relief organizations.
Top 10 Reasons to Become a Dentist
- Serve Others: Help people maintain and improve their oral health, quality of life and appearance
- Balance Your Lifestyle: Dentistry offers flexibility to balance professional and personal life
- Empower Your Patients: Give patients smiles they are proud to wear
- Research: Be involved with the scientific advancement of dentistry
- Be a Leader: Earn respect from your family, friends and community
- Educate: Be an educator on the importance of oral health
- Detect Disease: Treat oral health and detect disease - including cancer and cardiovascular disease
- Be Creative: Merge your artistic and scientific talents
- Succeed: With the aging population and increase in access to care, the demand and need for dentistry is on the rise
- Be Your Own Boss: Own a dental practice and set your own schedule
Why choose a NCDS Member Dentist?
The North Carolina Dental Society keeps members up to date on the latest scientific developments and recommendations from the American Dental Association, Centers for Disease Control and Prevention, and the NC Occupational Safety and Health Administration.
While North Carolina dentists are required to attend 15 hours of certified continuing education each year for re-licensure, the North Carolina Dental Society provides a wide range of educational programming annually at seminars throughout the state and encourages its members to attend more than the state-required hours.
When you choose a NCDS/ADA member dentist, you’re choosing a dentist who has agreed to the ADA Principles of Ethics and Code of Professional Conduct. Every NCDS/ADA member dentist makes a professional promise to put your health and well-being first, and is committed to dealing with you ethically and honestly. The ADA Code is an essential part of your doctor-patient relationship. And it’s a core part of who we are as NCDS/ADA member dentists.
Learn more about the ADA Principle of Ethics and Code of Professional Conduct at MouthHealthy.org/ADAmember.
